In 2022, our lives were turned upside down. Our little girl, Klaudia, just shy of three and a half years old, had always been cheerful, playful, and full of the curiosity that fills every preschooler’s day. She loved her toys, her friends, and the simple joys of childhood. And then, in a sudden, devastating moment, everything changed.
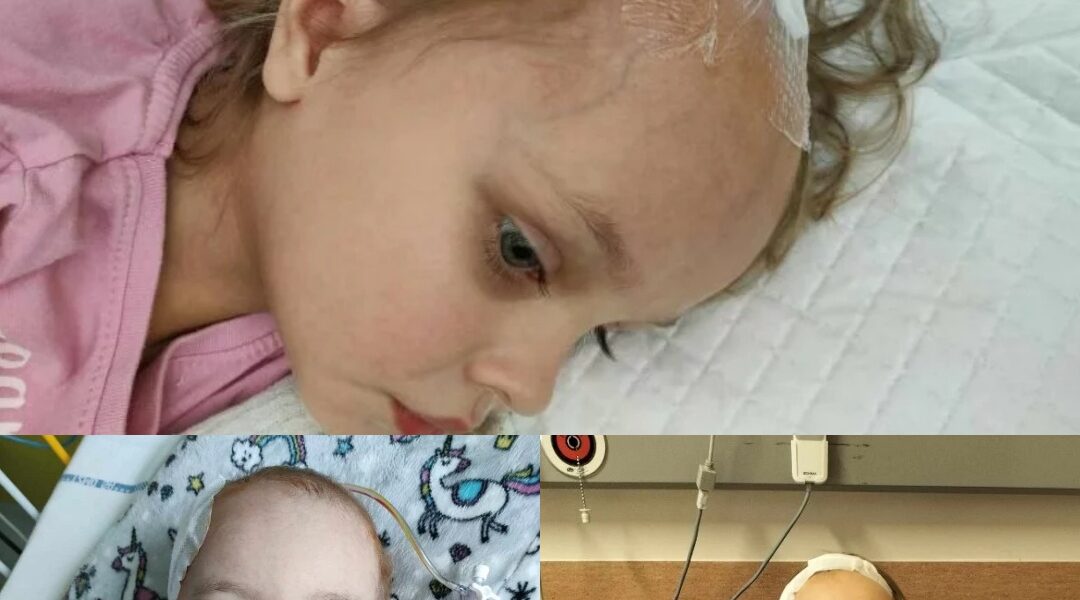
Klaudia began to lose her strength. She developed severe headaches, persistent vomiting, and strange changes in her vision — one eye strayed from focus, and her eyelid drooped. The panic and fear that consumed us as parents were indescribable. We rushed her to the hospital, and after tests, we received the words no parent ever wants to hear: she had a 6 x 4.5 x 4 cm polomyxoid astrocytoma, a rare and dangerous brain tumor. It was located at the border of the right thalamus and third ventricle, infiltrating crucial areas of her brain, including the right globus pallidus and hypothalamus. Hydrocephalus had developed because the tumor blocked the flow of cerebrospinal fluid, putting her delicate brain under immense pressure.

The journey that followed was unimaginably painful. Over three months in the hospital, Klaudia underwent five head surgeries and two external ventricular drainage procedures. For 32 days, she remained bedridden, relearning to walk each step at a time after these grueling operations. Despite the skill of her surgeons, only a partial resection was possible. A ventriculoperitoneal shunt was inserted to drain excess fluid, but complications were relentless. A week later, Klaudia developed a fever and severe abdominal pain; the shunt had become infected and had to be removed. She endured another month in the hospital, further surgery, treatments for the infection, and two additional weeks of bed rest. Finally, after such an ordeal, she left the hospital without a shunt, returning home on her own, though fragile and scarred by months of relentless struggle.
For less than a year, we believed we had survived the worst. Klaudia returned to some semblance of normalcy, attending preschool when possible, undergoing occasional endocrine and ophthalmological checkups, participating in rehabilitation, and enduring MRI scans every six months. We clung to hope. We dared to imagine that, despite everything, our little girl could still have a full, happy life.

But in 2023, the nightmare returned. The remaining tumor tissue began to grow, creating increased intracranial pressure and blocking the proper flow of cerebrospinal fluid. Klaudia could no longer cope without surgical intervention, and the shunt had to be reinserted. She returned to preschool and her everyday activities once again, though the shadow of her condition never truly left us.
Over time, we sought every available avenue for help. We consulted doctors across Poland and reached out to parents of children with the same rare tumor, searching for answers and solutions. Sadly, the tumor’s location is exceptionally delicate, too risky for her neurosurgeons to access fully. Every scan, every doctor visit, brought new anxiety, as we faced the cruel reality that her tumor could continue growing unchecked.
Recently, Klaudia underwent her sixth surgery — a staggering number for such a tiny head. Once again, the operation was only partially successful; as the doctors said, they did what they could “within reason.” The surgery was essential to prevent further brain damage, epilepsy, and the progressive paralysis that threatened her mobility and independence. The road ahead is long and uncertain, but her parents remain steadfast.
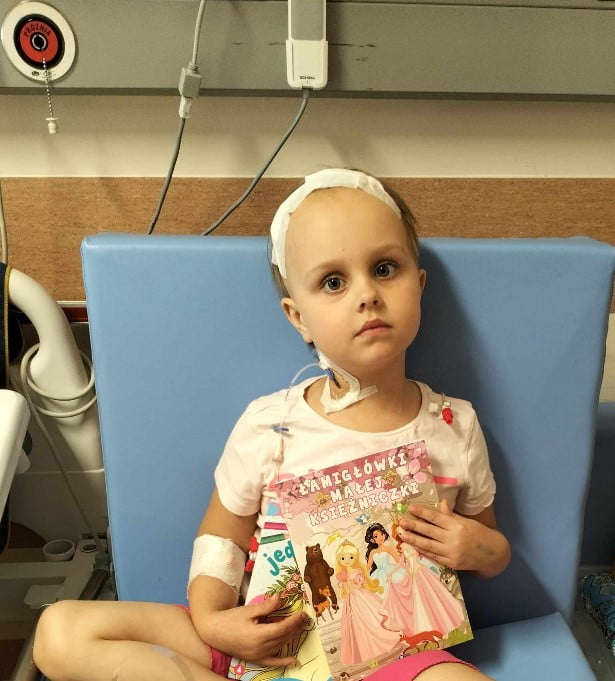
We are holding onto every ounce of hope and strength we have. We believe that complete removal of the tumor is possible — and that Klaudia deserves a life free from fear, pain, and limitation. Every day, we see her resilience, her courage, and her determination to reclaim the childhood that the illness has stolen from her. Her laughter, her curiosity, and her simple joys remind us why we fight.
But this fight cannot be fought alone. Klaudia requires not only expert surgical care, but also intensive rehabilitation, constant monitoring, and long-term therapy to support her recovery. Every step, every therapy session, every supportive intervention brings her closer to the life she deserves. And every effort requires resources that are beyond our reach.

Our plea is simple: help Klaudia live. Help her have the chance to run, to learn, to play, to dream — to experience the same joys that should be the right of every child. Every act of kindness, every donation, every shared story helps carry her one step closer to healing.
Klaudia is not just a patient; she is our daughter, our joy, and our inspiration. Her brother, her family, and everyone who loves her are standing beside her in this fight. Together, we believe that her courage, combined with the generosity and support of others, can turn a seemingly impossible battle into hope realized.

For Klaudia, every day matters. Every opportunity for treatment matters. Every gesture of support matters. And with your help, we can give her a chance to live fully, freely, and joyfully — as every child deserves.
Parents and Brother
Julian: Half a Heart, a Full Life, and Endless Courage.3285

When Julian was still living carefree in my heart, and I was walking with my almost three-year-old son, people would ask with sympathy, “Will it be a boy or a girl?” When I answered that it was a second son, the most common response I heard was, “Oh, but the most important thing is that it’s healthy!” And I already knew how important that thing wouldn’t happen for us.
Julian is a joyful and curious boy, almost two years old. Unfortunately, fate was stingy with him from the start, giving him only half a heart. In June 2016, we learned that our second son wouldn’t be like other children, like his older brother.
The mid-term scan was not a joyful, playful sight. It was an attempt to detect the red dots on the ultrasound monitor, signaling that blood was flowing into the left ventricle of the heart, and that it was working. Unfortunately, the flow was minimal, and the ventricle wasn’t working as it should.
All the abnormalities pointed to one thing: the most severe congenital heart defect, hypoplastic left heart syndrome (HLHS). A critical, incurable defect. Our world collapsed in a matter of minutes.
A very winding road lay before us, one that only we knew about. For our son to live, he required at least three stages of palliative surgical treatment. Julian had to be born in a hospital where a team of specialists would begin fighting for his life immediately after birth.

He spent only 15 minutes in my arms, then was placed in an incubator for long days and nights, hooked up to continuous infusions, wires, and cables. Doctors had to use medications to maintain fetal circulation so that Julian could survive until his first surgery.
During our pregnancy, we were fortunate that our doctor detected the heart defect early, for which we will be forever grateful. He was the first to give Julian a second life. Not all parents are so lucky.
Looking at our newborn, no one would ever have guessed he was terminally ill and would soon die without help. He was a large, robust, full-term boy, weighing 3930 grams, measuring 59 centimeters, and scored a full 10 on the Apgar scale. He barely fit in the incubator.
The birth of a child is a life-altering experience for the entire family. Shifting priorities and not enough hours in the day are probably what the average parent of a newborn experiences. It was similar for us, but on a more elevated level.
Julian’s performance declined with each passing day, his parameters were dropping, and his condition was classified as moderately severe. Every day, as visiting hours passed, I said goodbye to him, unsure if he would live to see the next day. The doctors offered no comfort; they simply told us how it was.
Finally, after almost a week, we were asked to sign the consent form for the first surgery. Without a doubt, it was one of the most difficult days of our lives. While signing the documents, we were informed of the risks and the difficulty of the surgery.

We knew once again that Julian was terminally ill, and the congenital HLHS defect could not be corrected or cured. His heart would never function like a healthy heart. The first stage of palliative treatment carries the highest mortality rate, and we didn’t know if he would survive.
After a difficult moment, we went to the hospital chaplain to ask for his Baptism. In the darkness, illuminated only by the heart monitors and small lights at the children’s stations, we prayed for Julian and reaffirmed our commitment through the familiar ceremony of receiving Holy Baptism. Moments later, we had to say farewell to our warrior and disappear behind the door.
The next day, zero hour struck. Julian was rushed to the operating room. Every second of waiting for information felt like an eternity. When we finally received the news that the operation was complete, we were told he had been brought out of general hypothermia and was stable, though connected to a specially designed device to maintain circulation.
Relief was long in coming. Julian now had to channel all his strength into the fight for life. The next few days were crucial. An open incubator, ventilator, drains, tubes, cables, pumps, syringes, and the intermittent beeping of the heart monitor alarm surrounded him.

We drew strength from our deepest reserves to support our warrior and his older brother, who tried to understand little. Each day, we drove the familiar route to the hospital, watching over Julian and squeezing every minute of our short visiting hours. We waited for him to start peeing, to tolerate food, to come off the ventilator, and to taper off his medication. Step by step, he moved forward.
After the first stage, Julian spent 26 days in the hospital. The day he went home was unforgettable. Our three and a half hearts were bursting with joy and pride.
Three months later, during a second checkup, we learned that the aortic stenosis had returned. Immediate cardiac catheterization was required. The balloon dilation was unsuccessful, so the doctors inserted a stent.
Months later, Julian returned for the third stage of surgery. Waiting in the intensive care unit for news about the operation was excruciating. When we finally saw him, swollen and attached to familiar equipment, our hearts shattered. He had grown, become stronger, but the battle was far from over.
Four days later, he was transferred to the cardiac surgery ward. Though he was with me 24/7, the postoperative period was very difficult. Oral medications were hard to tolerate, appetite was poor, and pumps and syringes restricted movement. Only intravenous painkillers brought relief.
After more than a week, treatment began to show effect, and Julian slowly returned to himself. Twenty days after surgery, he was cleared to go home. The reunion with his older brother brought tears of joy.

The third stage of palliative surgery remains essential for Julian’s survival. Without it, he cannot live. Professor Edward Malec from the Muenster Clinic has agreed to perform the operation. Thanks to generous donors, the full amount needed for surgery in Germany has been collected — approximately 170,000 złoty.
Julian’s treatment also involves medications, medical equipment, and specialist visits. After the third surgery, his blood clotting will need constant monitoring, requiring special devices and ongoing care. Travel, hotel accommodations, and perioperative expenses are additional challenges.
Julian will never have a healthy heart, but he wants to live and grow like other children. He may only have half a heart, but his will to fight and zest for life are more than whole. Every day he inspires us, reminding us that courage and hope can survive even the most difficult circumstances.